
Data with depth.
Results with relevance.®
Ultra-sensitive MRD Detection
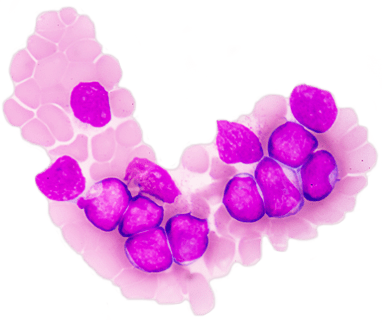
clonoSEQ® Assay is a highly sensitive, specific, and standardized method for detecting and monitoring MRD, in B-cell lymphoid malignancies. MRD refers to the small number of cancer cells that can remain in a patient’s body after treatment and may eventually cause recurrence of the disease.
clonoSEQ leverages the power of next-generation DNA sequencing (NGS) and offers an accurate and reliable way to assess how disease burden changes over time in response to treatment or during remission.[1] clonoSEQ can help clinicians:
What gets measured gets managed®
clonoSEQ detects residual disease by identifying the individual DNA sequences associated with lymphoid cancers. Once identified in a high disease load diagnostic or relapse sample, these sequences can be tracked over time, allowing clinicians to monitor the patient’s disease status in follow-up samples throughout the course of treatment and during remission.[1]
clonoSEQ provides more than a binary (yes/no) assessment of the presence of disease.[1] The assay quantifies residual disease, tracks the identified sequences over time, and monitors for the emergence of new sequences, which may signal disease evolution or recurrence. The deep sensitivity of the clonoSEQ Assay has been shown to help predict patient outcomes and add insight to the evaluation of disease response to therapy, enabling timely decisions about how and when to intervene.
During Treatment:
CONFIDENTLY MONITOR RESPONSE
During Remission:
DETECT POTENTIAL RELAPSE
Meaningful advantages of the clonoSEQ Assay for residual disease detection and monitoring
The clonoSEQ Assay leverages the power of immunosequencing coupled with groundbreaking advances in chemistry and proprietary bioinformatics to assess the presence of malignant cells at levels below the detection limit of conventional cytomorphological methods.[2] When a sufficient sample is provided, the assay can routinely identify the presence of one cancer cell in a sample of 1 million healthy cells.[1]
Sensitivity
clonoSEQ detects measurable residual disease (MRD) at the level of a single cancer cell among a million cells, given sufficient sample input.[1] The assay provides a continuous measure of MRD, with its sensitivity limited only by the amount of DNA analyzed.[1] Measuring MRD at such low levels offers prognostic value to clinicians as they assess how patients respond to treatment.[1]
Specificity
clonoSEQ enables identification and tracking of individual cancer cells. Once the DNA sequences associated with these cancer cells are identified, the presence of each specific sequence can be assessed in subsequent MRD samples, enabling clinicians to gain a more precise understanding of disease burden over time.[1]
Standardization
clonoSEQ has undergone extensive analytical and clinical validation, fulfilling requirements for FDA clearance for in vitro diagnostic use.[1] The consistency demonstrated across these validation studies meets the high bar for standardization required by cooperative research groups and drug developers, while also enhancing patient management in the clinic.
MRD testing is recommended by clinical practice guidelines
MRD assessment is recognized as an essential metric to inform and enhance treatment decisions throughout treatment in a growing number of lymphoid malignancies. International clinical practice guidelines recommend assessing MRD at multiple time points during treatment and maintenance in CLL, multiple myeloma, and B-ALL, and include NGS as a testing method option.[3,6]
MULTIPLE MYELOMA
NCCN Clinical Practice Guidelines In Oncology (NCCN Guidelines®) incorporate MRD testing as a Category 2A recommendation for myeloma patients.[3]

International Myeloma Working Group (IMWG) Criteria[7]

ACUTE LYMPHOBLASTIC LEUKEMIA
NCCN Guidelines® incorporate MRD testing as a Category 2A recommendation for patients with ALL.[4,5]

CHRONIC LYMPHOCYTIC LEUKEMIA
NCCN Guidelines® incorporate MRD testing as a Category 2A recommendation for patients with CLL.[6]

Contact Us
Make an inquiry to learn more about our products.
Citations
- The clonoSEQ Assay B-Cell Reagent Set is CE marked as in vitro diagnostic (IVD) for assessing the MRD status and changes in disease burden during and after treatment in B-Cell malignancies in DNA extracted from blood and/or bone marrow samples.
- Sherrod A, et al. Bone Marrow Transplant. 2015;51:2-12.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Multiple Myeloma V.3.2020. © National Comprehensive Cancer Network, Inc. 2020. All rights reserved. Accessed March 11th, 2020. To view the most recent and complete version of the guideline, go to NCCN.org.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Pediatric Acute Lymphoblastic Leukemia V.2.2020. © National Comprehensive Cancer Network, Inc. 2020. All rights reserved. Accessed March 11th, 2020. To view the most recent and complete version of the guideline, go to NCCN.org.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Acute Lymphoblastic Leukemia V.1.2020. © National Comprehensive Cancer Network, Inc. 2020. All rights reserved. Accessed March 11th, 2020. To view the most recent and complete version of the guideline, go to NCCN.org.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Chronic Lymphocytic Leukemia/Small Lymphocytic Leukemia V.4.2020. © National Comprehensive Cancer Network, Inc. 2020. All rights reserved. Accessed [February 19, 2020]. To view the most recent and complete version of the guideline, go online to NCCN.org.
- Kumar S, et al. Lancet Oncol. 2016;17(8):e328-46.
*NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
