Multiple Myeloma FDA-cleared in bone marrow, CLIA-validated in peripheral blood
clonoSEQ delivers actionable answers that inform personalized treatment decisions
Complete response isn’t the complete picture
Because most patients who achieve a CR eventually relapse, clonoSEQ can provide additional information to support care plans1-4
All about actionability
Emerging data are advancing the case for using clonoSEQ results to help guide treatment decisions5,6
clonoSEQ is convenient
clonoSEQ blood testing supports serial MRD monitoring as a potential alternative to frequent marrow draws
Clinical practice guidelines and clinical trial experience support MRD monitoring at multiple timepoints5-9
| Clinical practice guidelines |
Clinical trial experience |
|
|---|---|---|
| Induction | ||
| Transplant | ||
| Consolidation |
|
|
| Maintenance |
|
|
Post-induction MRD status provides predictive value beyond CR
82%vs49%
5-year PFS for MRD negative patients with CR vs patients in CR but still MRD positive8
88%vs78%
5-year OS for MRD-negative patients with CR vs patients in CR but still MRD positive8
NCODA PQI for MRD testing in multiple myeloma:
A straightforward overview of how to use MRD testing in clinical practice
clonoSEQ provides greater insights than disease stage or cytogenetics
In newly diagnosed MM patients receiving maintenance therapy, MRD negativity was the strongest predictor of PFS10
MRD status more effectively predicted outcomes than traditional risk factors, irrespective of:
clonoSEQ provides insights that can support your transplant decision
In the DETERMINATION trial, PFS was similar for MRD-negative patients regardless of transplant
Emerging data show why you might consider personalizing treatment decisions based on MRD status in the maintenance setting
In the MASTER trial, there was low 1-year progression for most patients who stopped treatment based on 2 MRD-negative tests
Real-world evidence shows the benefit of using MRD positivity to intensify or modify treatment
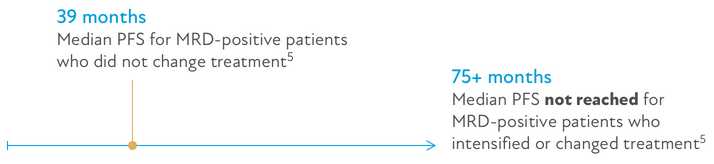
Our results suggest that the use of MRD to make clinical decisions has a positive impact on survival outcomes.
-Martinez-Lopez et al5
View real-world case studies that informed care
Dr. Susan Bal
MRD Helps Predict Outcomes and Informs Maintenance Treatment
Dr. Rafael Fonseca
MRD-Informed Treatment Decisions in the Relapsed Setting
Dr. Rafael Fonseca
Individualizing Transplant Decisions Based on Depth of Response
Higher Sensitivity
clonoSEQ detects disease that MFC cannot
Percentage of patients who were MRD negative by MFC but had residual disease by clonoSEQ11
ASCT, autologous stem cell transplants; CR, complete response; ISS, international staging system; MFC, multiparameter flow cytometry; NDMM, newly diagnosed multiple myeloma; NGS, next-generation sequencing; OS, overall survival; PFS, progression-free survival; RVd, lenalidomide + bortezomib + dexamethasone.
About the studies
Induction
Martinez-Lopez et al assessed bone marrow samples from 62 myeloma patients who achieved a complete remission after frontline therapy in studies using the GEM2000, GEM05, or GEM10 protocols (n = 133). Samples were assessed for MRD after induction therapy; <10-5 was defined as MRD negative by Adaptive’s NGS Assay.8
Transplant
DETERMINATION was a phase 3 trial evaluating RVd alone or RVd + ASCT in patients with NDMM (n = 357). MRD was assessed by clonoSEQ (10-5) from the start of lenalidomide maintenance therapy in 108 patients in the RVd-alone group and 90 patients in the RVd + ASCT group. In the IFM2009 study, 509 newly diagnosed MM patients received RVd +/- transplant followed by 12 months of lenalidomide maintenance therapy. An analysis of the 239 patients with known MRD status after completion of maintenance therapy was performed to determine whether cytogenic risk or ISS stage modifies the relationship between MRD and outcomes.9
Maintenance MRD-negative
MASTER was a multicenter, single-arm, phase 2 trial of patients with NDMM, conducted by Costa et al. Patients received Dara-KRd induction, ASCT, and Dara-KRd consolidation, according to MRD status. MRD was evaluated by NGS at the end of induction, post-ASCT, and every 4 cycles (maximum of 8 cycles) of consolidation. Primary endpoint was achievement of MRD negativity (10-5). Subjects with 2 consecutive MRD-negative assessments entered treatment-free MRD surveillance.6
Maintenance MRD-positive
In a retrospective review of 400 patients with NDMM and relapsed/refractory multiple myeloma who had at least 1 MRD assessment, Martinez-Lopez et al explored how clinical decisions made based on MRD results affected outcomes. MRD was assessed by MFC or clonoSEQ with sensitivity from 10-5 to 10-6. Treatment intensification or change was made during maintenance therapy in 83% of subjects.5
clonoSEQ vs MFS
In the IFM 2009 study, patients at pre-maintenance and post-maintenance timepoints who were identified as MFC MRD negative (10-4) were assessed by clonoSEQ (10-6). Of these patients, 84 and 42, respectively, were identified as MRD positive.11
This page is intended for a US-based audience.
clonoSEQ® is available as an FDA-cleared in vitro diagnostic (IVD) test service provided by Adaptive Biotechnologies to detect minimal residual disease (MRD) in bone marrow from patients with multiple myeloma or B-cell acute lymphoblastic leukemia (B-ALL) and blood or bone marrow from patients with chronic lymphocytic leukemia (CLL). CLL Clonality (ID) Tests will also produce an IGHV status result, which is provided as a CLIA-validated laboratory developed test (LDT) but which has not been cleared or approved by the FDA. Additionally, clonoSEQ is available for use in other lymphoid cancers and specimen types as a CLIA-validated LDT. For important information about the FDA-cleared uses of clonoSEQ including test limitations, please visit clonoSEQ.com/technical-summary.
References
- Lahuerta JJ, et al. J Clin Oncol. 2017;35(25):2900-2910.
- San-Miguel J, et al. Blood. 2021;139(4):492-501.
- Cavo M, et al. Blood. 2022;139(6):835-844.
- Cedena MT, et al. PLoS ONE. 2020;15(8):e0237155.
- Martinez-Lopez J, et al. J Hematol Oncol. 2021;14(1):126.
- Costa LJ, et al. J Clin Oncol. 2021;JCO2101935.
- Referenced with permission from the NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®) for Multiple Myeloma V.5.2022. © National Comprehensive Cancer Network, Inc. 2021. All rights reserved. Accessed July 1, 2022. To view the most recent and complete version of the guideline, go online to NCCN.org. NCCN makes no warranties of any kind whatsoever regarding their content, use or application and disclaims any responsibility for their application or use in any way.
- Martinez-Lopez J, et al. Blood. 2014;123(20):3073-3079.
- Richardson PG, et al. N Engl J Med. 2022;387(2):132-147.
- Perrot A, et al. Blood. 2018;132(23):2456-2464.
- Avet-Loiseau H, et al. Blood. 2015;126(23):191.
