NEW: Updated NCCN MM Guidelines Strengthen Recommendation for Baseline Clonotype ID at Diagnosis.
Covered by Medicare and FDA-cleared, clonoSEQ supports baseline ID assessment to enable subsequent next generation sequencing (NGS)-based MRD tracking. For more info about incorporating clonoSEQ into your clinical practice for MM patients, click here.
Adaptive Assist™
Helping patients access the clinical insights of clonoSEQ MRD testing
How we support patient access to clonoSEQ testing
- Upfront, out-of-pocket (OOP), and Good Faith cost estimates
- Prior authorization management
- Assistance with out-of-pocket costs for qualifying patients
- Appeal for maximum benefits and lowest out-of-pocket costs
90%
of patients have no OOP costs for clonoSEQ testing*
*Prior to enrolling in the Adaptive Assist Patient Financial Assistance Program
Covered by Medicare and the largest national private insurers
Streamline Prior Authorization (PA) Management with our PA vendors
While Adaptive manages PAs for clonoSEQ orders, some insurance companies do not allow the rendering lab to do so. In these instances, Adaptive partners with Careviso and Glidian, third party companies, that submit and track PAs on a provider’s behalf.
- Faster prior authorization responses
- Fewer denials and cancellations
- Fewer inbound calls for you and your staff to manage
- Improved coverage outcomes for clonoSEQ testing
Providers can register directly with Glidian at my.glidian.com/provider. To register with Careviso by contacting our Sr. Reimbursement Account Specialists at clonoSEQRAS@adaptivebiotech.com.
Adaptive Assist resources
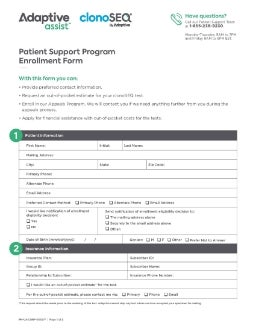
Adaptive Assist Patient Financial Assistance Program Application
Adaptive Assist Patient Financial Assistance Program Application

Adaptive Assist Program Brochure with FAQs
Adaptive Assist Program
Brochure
Frequently asked questions
Is the clonoSEQ® Assay covered by commercial insurance?
Adaptive Biotechnologies (Adaptive) has in-network contracts with most major national payers and accepts all insurances for clonoSEQ testing. Adaptive will bill a patient’s insurance company directly and will work with your patient’s plan to obtain the proper level of coverage for clonoSEQ. 90% of patients have no out-of-pocket (OOP) costs. For patients who have an OOP cost for testing, Adaptive Assist provides a variety of payment assistance options for qualified patients that will fit the patient’s individual financial circumstance.
Is clonoSEQ testing covered by Medicare?
Medicare covers clonoSEQ testing performed on blood or bone marrow samples from patients with multiple myeloma, B-cell acute lymphoblastic leukemia, chronic lymphocytic leukemia, or diffuse large B-cell lymphoma, at multiple time points throughout a patient’s treatment. If the testing does not meet the above criteria an Advanced Beneficiary Notice (ABN) should be completed informing patients that Medicare considers the testing to be
noncovered.*
*Full coverage policy details for clonoSEQ can be accessed at the CMS website at https://go.cms.gov/2GL4Ej5. Please refer to www.clonoseq.com/resources-and-support/downloadable-resources for more information or to download an ABN template.
What if my patient’s insurance requires a prior authorization?
Adaptive will evaluate all incoming clinical orders to assess for the need of a prior authorization. If one is needed and Adaptive can submit for one, we will do so. If the insurance company requires the referring physician’s office to submit, our team will reach out to your office staff with guidance on how to submit for a prior authorization.
- Adaptive works with a third party to obtain physician-initiated prior authorizations. If you are interested in signing up for this service, please call our Patient Support hotline at 1-855-236-9230 for more information
Can I find out what my patients’ potential out-of-pocket costs for the test will be?
Out-of-pocket cost estimates are available prior to submission of a clonoSEQ order by contacting our Patient Support Team at 1-855-236-9230. The amount quoted during this process is an estimate based on plan benefits and unmet deductible or coinsurance and/or copay amounts and is subject to change based on other claims that are being processed for your patient. During the call, we will attempt to qualify eligible patients for financial assistance through our Adaptive Assist Patient Support Program. Patients who qualify for financial assistance will have no OOP costs for a year from qualification date.
The caller will need to have the patient’s insurance information on hand. To obtain estimates for multiple patients at one time, please send the patients’ insurance via fax to 1-206-299-0488.
- Please note that we cannot stop testing on samples that have been received and accepted by Adaptive
What happens if a patient’s insurance limits or denies payment for clonoSEQ testing?
In the event that coverage for clonoSEQ is limited or denied, Adaptive will help appeal the claim when possible and work on behalf of the patient to seek payment for clonoSEQ testing services. Adaptive may require support from you and your office in the appeals process. We greatly appreciate your partnership in this process on behalf of your patients.
What documentation is needed from physicians and/or their offices to support clonoSEQ appeals?
In many cases, Adaptive will have the information required to submit an appeal on behalf of a patient. Where possible, Adaptive will work to limit the effort required by you and your office to support the appeals process. However, for certain types of appeals, insurance companies may require additional information and records, including:
- A Letter of Medical Necessity (LOMN) signed by the ordering physician. If an LOMN is required, Adaptive will notify physicians via the clonoSEQ Diagnostic Ordering Portal
- Clinic note(s) associated with a patient visit related to the clonoSEQ order
- Medical records including clinical history, treatment plans, and notes
If patient consent is required for an appeal, Adaptive will send a consent form along with a letter to the patient briefly explaining the need for consent and will follow up accordingly.
What if my patient received a bill for clonoSEQ testing and cannot afford the payment?
The Adaptive Assist Patient Support Program offers a variety of options to meet each patient’s unique financial circumstances. Patients can call the Patient Support Team at 1-855-236-9230 to discuss their individual financial circumstances and the assistance options available to them if they qualify.
What are the patient eligibility criteria to qualify for financial assistance?†
To be eligible for financial assistance, a patient must meet all of the following criteria:
- Be a US citizen or legal resident age 18 years or older
- Patients under the age of 18 are eligible but require the application form to be signed by a parent or legal guardian
- Be uninsured or have insurance that does not cover the full cost of clonoSEQ testing
- Meet financial need requirements based on the patient’s income and the number of persons in their household, or the sum of medical expenses as a percentage of household income
†The Adaptive Assist Patient Support Program is subject to change at the discretion of Adaptive.
How does a patient apply for financial assistance for clonoSEQ testing?
For new or existing clonoSEQ patients, applying for financial assistance is designed to be a straightforward and transparent process.
- Patients can call 1-855-236-9230 to discuss their insurance and individual financial circumstances in order to better understand their potential financial responsibility for clonoSEQ testing. Patients are able to qualify and enroll for financial assistance during this phone call. Alternatively, a patient can download an application to complete and send in by visiting Adaptive-Assist.com
- If selected for the upfront enrollment verification process, a patient will be notified of the need to submit supporting documentation (e.g. tax return, W-2, pay stub and, if applicable medical bills, medication and/or test receipts) within 45 days
What if a patient has a question about a statement from Adaptive or an Explanation of Benefits (EOB) that they received from their insurance company for clonoSEQ testing?
For questions about billing, payment options, insurance coverage, or assistance, patients can call the Patient Support Team at 1-855-236-9230. Representatives are available Monday through Thursday, 9 am to 7 pm ET and Friday, 9 am to 6 pm ET.
Need more help?
Speak to one of our expert Patient Support Team members to get answers to your questions.
Call 1-855-236-9230
Monday through Thursday, 9 am to 7 pm ET Friday, 9 am to 6 pm ET
This page is intended for a US-based audience.
clonoSEQ® is available as an FDA-cleared in vitro diagnostic (IVD) test service provided by Adaptive Biotechnologies to detect measurable residual disease (MRD) in bone marrow from patients with multiple myeloma or B-cell acute lymphoblastic leukemia (B-ALL) and blood or bone marrow from patients with chronic lymphocytic leukemia (CLL). Additionally, clonoSEQ is available for use in other lymphoid cancers and specimen types as a CLIA-validated laboratory developed test (LDT). To review the FDA-cleared uses of clonoSEQ, visit clonoSEQ.com/technical-summary.